When Darkness Meets Light: Understanding the Complex World of Bipolar Depression
When Darkness Meets Light: Understanding the Complex World of Bipolar Depression
Sarah stared at her ceiling at 3 AM, wondering how she'd gone from organizing three charity events last month to barely managing to shower this week. The stark contrast wasn't just confusing—it was exhausting. Like millions of others living with bipolar disorder, she was navigating the treacherous waters of bipolar depression, a condition that's far more complex than many people realize.
The Two Faces of Mood: What Sets Bipolar Depression Apart
Most people think they understand depression. The persistent sadness, the loss of interest in activities, the overwhelming fatigue—these symptoms have become part of our cultural vocabulary. But bipolar depression carries an additional weight: the shadow of its opposite.
When someone experiences bipolar depression, they're not just dealing with low mood. They're grappling with a condition that can swing between devastating lows and potentially destructive highs. This isn't simply having "good days and bad days"—it's living with a brain that operates on extremes.
The depression phase in bipolar disorder often feels more intense than unipolar depression. Why? Because the contrast is so stark. Imagine running a marathon at top speed, then suddenly hitting a wall. That's what transitioning from a manic or hypomanic episode into depression can feel like. The energy that once seemed limitless evaporates, leaving behind a void that feels impossible to fill.
Breaking Down the Basics: Types and Patterns
Bipolar disorder isn't a one-size-fits-all diagnosis. Mental health professionals recognize several distinct patterns, each with its own rhythm of highs and lows.
Bipolar I disorder involves at least one manic episode—a period of abnormally elevated mood lasting at least a week, often accompanied by risky behavior, decreased need for sleep, and grandiose thinking. The depressive episodes in Bipolar I can be severe and long-lasting, sometimes stretching for months.
Bipolar II disorder might seem "milder" because it involves hypomania rather than full mania, but don't let that fool you. The depressive episodes in Bipolar II are often more frequent and can be just as debilitating. In fact, people with Bipolar II typically spend more time in depression than those with Bipolar I.
Then there's cyclothymic disorder, where mood swings are less severe but more constant—like living on an emotional seesaw that never quite stops moving. And rapid cycling? That's when someone experiences four or more mood episodes in a single year, creating a dizzying pattern of ups and downs that can leave both the person and their loved ones feeling perpetually off-balance.
The Hidden Struggle: Why Bipolar Depression Often Goes Unrecognized
Here's something that might surprise you: bipolar depression is frequently misdiagnosed as major depressive disorder. The reasons are frustratingly simple. When someone seeks help during a depressive episode, they're focused on their current suffering. They might not mention—or even remember clearly—previous manic or hypomanic episodes.
Think about it. If you're drowning in depression, are you likely to tell your doctor about that time six months ago when you felt amazing, stayed up for three nights straight redecorating your apartment, and maxed out your credit cards? Probably not. You're there because you feel terrible now.
This misdiagnosis matters more than you might think. Treating bipolar depression with standard antidepressants alone can trigger manic episodes or rapid cycling, potentially making the condition worse. It's like trying to fix a complex electrical problem by only addressing the blown fuse—you might temporarily restore power, but you haven't solved the underlying issue.
Inside the Mind: What Bipolar Depression Really Feels Like
Let me paint you a picture of bipolar depression through the eyes of those who live it. It's waking up feeling like gravity has tripled overnight. Every movement requires enormous effort. Your thoughts move through molasses, and simple decisions—what to wear, what to eat—become overwhelming obstacles.
But unlike unipolar depression, there's often an added layer of grief. People with bipolar disorder remember what it feels like to have boundless energy, crystal-clear thoughts, and unshakeable confidence. The contrast makes the depression feel even more suffocating. It's not just feeling bad—it's remembering feeling invincible and wondering if you'll ever feel that way again.
There's also the exhaustion that comes from mood cycling itself. Your brain and body aren't designed to handle such extreme fluctuations. It's like being a car that's constantly switching between fifth gear and reverse—eventually, something's going to wear out.
Many people describe a particular kind of mental fog during bipolar depression. Words slip away mid-sentence. Concentration becomes impossible. Work tasks that were simple last month now feel like climbing Everest. This cognitive impairment isn't just frustrating—it can be genuinely frightening, especially for people whose careers depend on mental sharpness.
The Biological Blueprint: Understanding the Brain in Bipolar Depression
Scientists have made remarkable progress in understanding what happens in the brain during bipolar disorder. Advanced imaging studies reveal differences in brain structure and function that help explain the mood swings.
The prefrontal cortex—your brain's CEO, responsible for decision-making and emotional regulation—shows altered activity in bipolar disorder. During depression, this area often becomes underactive, contributing to the difficulty in making decisions and the overwhelming nature of negative emotions.
Meanwhile, the amygdala, your brain's alarm system, tends to be overactive during both manic and depressive episodes. This hyperactivity might explain why emotions feel so intense and overwhelming during mood episodes.
Neurotransmitters—the chemical messengers in your brain—also play a crucial role. Serotonin, dopamine, and norepinephrine levels fluctuate dramatically in bipolar disorder. But it's not as simple as "low serotonin equals depression." The relationships between these chemicals are intricate, and their interactions with mood-regulating systems in the brain create the complex patterns we see in bipolar disorder.
Genetics definitely play a role too. If you have a first-degree relative with bipolar disorder, your risk increases significantly. But genes aren't destiny—they're more like risk factors that interact with environmental triggers and life experiences.
The Treatment Puzzle: Finding What Works
Managing bipolar depression requires a different approach than treating unipolar depression. It's not just about lifting mood—it's about stabilizing it. This typically means mood stabilizers form the foundation of treatment, with other medications added carefully and strategically.
Lithium, despite being one of the oldest psychiatric medications, remains a gold standard for many people. It's particularly effective at preventing both manic and depressive episodes. But like all medications, it's not without side effects, and regular blood monitoring is necessary.
Anticonvulsants like lamotrigine have proven especially helpful for bipolar depression. Unlike some mood stabilizers that are better at preventing mania, lamotrigine shines in preventing depressive episodes. For many people, it's been a game-changer.
Atypical antipsychotics might sound scary—the name certainly doesn't help—but they've become important tools in treating bipolar depression. Medications like quetiapine and lurasidone can lift depression while also protecting against mania.
The medication journey is rarely straightforward. Finding the right combination often takes time, patience, and close collaboration with a psychiatrist. What works beautifully for one person might cause intolerable side effects in another. It's a process of careful experimentation, always balancing effectiveness against quality of life.
Beyond Pills: The Power of Psychotherapy
While medication often forms the backbone of bipolar disorder treatment, psychotherapy plays an equally vital role. But not just any therapy—specific approaches have proven most effective for bipolar depression.
Cognitive Behavioral Therapy (CBT) helps people identify and change thought patterns that contribute to mood episodes. For someone with bipolar depression, this might mean recognizing early warning signs of mood shifts and developing strategies to maintain stability.
Interpersonal and Social Rhythm Therapy (IPSRT) focuses on the connection between daily routines and mood stability. It turns out that maintaining regular sleep-wake cycles, meal times, and activity patterns can significantly impact mood stability in bipolar disorder. This therapy helps people create and stick to routines that support mental health.
Family-focused therapy acknowledges that bipolar disorder doesn't exist in a vacuum. It affects relationships, and relationships affect the course of the disorder. This approach helps both the person with bipolar disorder and their loved ones understand the condition better and develop healthy communication patterns.
Dialectical Behavior Therapy (DBT), originally developed for borderline personality disorder, has shown promise for bipolar disorder too. Its emphasis on emotion regulation and distress tolerance skills can be particularly helpful during mood episodes.
Living Day to Day: Practical Strategies That Make a Difference
Managing bipolar depression isn't just about professional treatment—it's about the dozens of small choices made every day. These lifestyle factors might seem simple, but their impact can be profound.
Sleep is perhaps the most critical factor. For people with bipolar disorder, sleep disruption can trigger mood episodes in either direction. This means prioritizing sleep hygiene isn't just good advice—it's essential medical management. Going to bed and waking up at consistent times, even on weekends, helps maintain mood stability.
Exercise presents an interesting challenge. During depression, it feels impossible. During hypomania, it might feel unnecessary. But regular, moderate exercise has proven mood-stabilizing effects. The key is finding sustainable activities that you can maintain across mood states.
Nutrition matters too, though not in the way diet culture might suggest. It's not about following the latest fad—it's about maintaining stable blood sugar levels and ensuring your brain has the nutrients it needs. Regular meals with balanced macronutrients can help prevent the energy crashes that worsen mood symptoms.
Stress management isn't optional when you have bipolar disorder. Stress is a known trigger for mood episodes, so developing effective coping strategies is crucial. This might include meditation, yoga, journaling, or simply learning to say no to overwhelming commitments.
The Social Dimension: Relationships and Bipolar Depression
Bipolar disorder doesn't just affect the person diagnosed—it ripples through their entire social network. During depressive episodes, maintaining relationships can feel impossible. The energy required for social interaction simply isn't there, and the guilt about being a "bad friend" or "distant partner" compounds the depression.
From the outside, bipolar depression can be bewildering for loved ones. They might struggle to understand how someone who was recently so energetic and engaged can suddenly withdraw completely. Without education about the condition, they might take this withdrawal personally or push for interaction in ways that feel overwhelming.
Communication becomes crucial but challenging. How do you explain that you care deeply about someone but can't muster the energy to return their texts? How do you help them understand that your isolation isn't about them—it's about the enormous effort required just to exist?
Many people with bipolar disorder find it helpful to have conversations about their condition during stable periods. Explaining the nature of mood episodes, discussing what helps and what doesn't, and even creating action plans for different mood states can strengthen relationships and reduce misunderstandings.
The Workplace Challenge: Career and Bipolar Depression
Navigating a career with bipolar disorder requires careful planning and often, difficult decisions about disclosure. The Americans with Disabilities Act provides protections, but stigma remains real, and not everyone feels safe being open about their diagnosis.
During depressive episodes, work performance inevitably suffers. Concentration problems, fatigue, and lack of motivation can make even routine tasks feel insurmountable. Some people find that flexible work arrangements—like the ability to work from home or adjust hours—can help them maintain employment through mood fluctuations.
The key is often in developing systems during stable periods that can sustain you through difficult times. This might mean detailed documentation of work processes, building in buffer time for projects, or cultivating a support network of trusted colleagues.
Some careers naturally accommodate mood fluctuations better than others. Creative fields, consulting work, or positions with seasonal variations might work well for some people. Others find that highly structured environments provide the external stability that helps maintain mood balance.
The Question of Creativity: Blessing, Curse, or Myth?
The link between bipolar disorder and creativity has fascinated researchers and the public alike. Many famous artists, writers, and musicians have lived with bipolar disorder, leading to romanticized notions about madness and genius.
The reality is more nuanced. Some people do experience enhanced creativity during hypomanic episodes—colors seem brighter, connections between ideas flow more freely, and creative output increases. But this comes at a cost. The depression that follows often erases any gains, and the overall instability can derail creative careers.
Moreover, the idea that treatment dampens creativity has kept some people from seeking help. While some medications can affect creative thinking, many people find that mood stability actually enhances their creative work. It's hard to produce great art when you're too depressed to get out of bed or too manic to focus on a single project.
The goal isn't to eliminate mood variations entirely—some fluctuation is normal and can indeed fuel creativity. Instead, it's about finding a sustainable range where creativity can flourish without the destructive extremes.
Hope in the Darkness: Recovery and Resilience
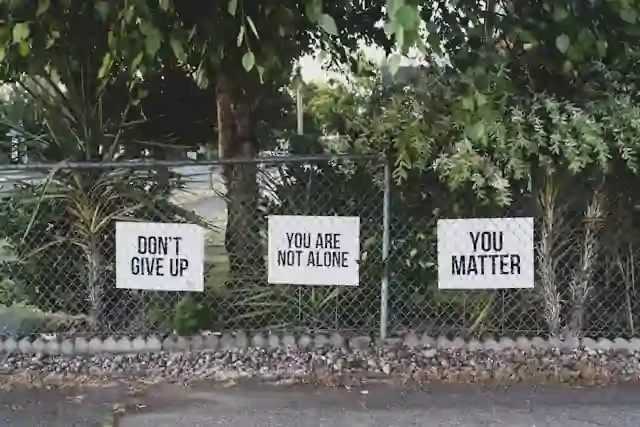
Here's what everyone living with bipolar depression needs to know: recovery is possible. Not cure—bipolar disorder is a chronic condition—but recovery in the sense of living a full, meaningful life.
Recovery looks different for everyone. For some, it means long periods of stability with occasional, manageable mood fluctuations. For others, it's about reducing the severity of episodes and bouncing back more quickly. The goal isn't perfection—it's progress.
Building resilience is an ongoing process. It involves developing a deep understanding of your own patterns, creating a robust support system, and maintaining treatment even when you feel well. It means celebrating small victories—getting through a day of work during depression, recognizing early warning signs of mood shifts, or simply maintaining hope during dark times.
Many people with bipolar disorder describe eventually reaching a place of acceptance—not resignation, but a genuine peace with their condition. They learn to work with their brain rather than against it, to recognize both the challenges and the unique perspectives that can come with bipolar disorder.
The Research Horizon: What's Coming Next
The field of bipolar disorder research is more active than ever. Scientists are exploring new treatment approaches that go beyond traditional medications. Ketamine and other rapid-acting antidepressants show promise for bipolar depression, potentially offering relief in hours or days rather than weeks.
Digital health tools are revolutionizing how people track and manage their moods. Smartphone apps can detect subtle changes in behavior—like typing speed or movement patterns—that might signal an impending mood episode. This early warning system could help people intervene before episodes become severe.
Researchers are also investigating the role of inflammation in bipolar disorder. Some studies suggest that anti-inflammatory treatments might help stabilize mood, opening up entirely new avenues for treatment.
Personalized medicine approaches are becoming more sophisticated. Genetic testing might soon help predict which medications are most likely to work for individual patients, reducing the trial-and-error period that can be so frustrating.
A Message of Understanding
If you're reading this while in the grip of bipolar depression, know that your struggle is real and valid. The exhaustion you feel isn't laziness. The fog in your mind isn't stupidity. The effort required for basic tasks isn't weakness. You're fighting a battle that many people can't see or understand, and you're braver than you know.
If you love someone with bipolar disorder, your patience and understanding make more difference than you might realize. Learning about the condition, offering support without judgment, and maintaining hope when they can't—these acts of love can be lifesaving.
The path forward with bipolar depression isn't straight. It winds, doubles back, and sometimes seems to disappear entirely. But it does lead somewhere. With each step—each medication adjustment, each therapy session, each day of maintaining healthy habits despite not wanting to—you build a life that's not defined by bipolar disorder but informed by the strength developed in managing it.
The darkness of bipolar depression can be profound, but it's not permanent. The light returns—different perhaps than before, but often appreciated in ways that those who've never experienced such darkness can't quite understand. In that appreciation, in that hard-won wisdom, many people with bipolar disorder find not just survival, but a particular kind of thriving that honors both the struggles and the strengths that come with this complex condition.
Living with bipolar depression means accepting a certain amount of uncertainty. But within that acceptance lies freedom—the freedom to stop fighting against your brain and start working with it, to stop seeing bipolar disorder as purely negative and start recognizing the resilience it's built in you, to stop waiting for a cure and start building a life worth living right now, mood swings and all.
The story of bipolar depression isn't ultimately about illness—it's about the remarkable human capacity to adapt, persevere, and find meaning even in the most challenging circumstances. It's about discovering that you're stronger than you ever imagined, that hope can coexist with struggle, and that a life touched by bipolar disorder can still be a life fully lived.
The Seasonal Connection: When Time of Year Matters
I remember the first time my psychiatrist asked if I'd noticed any patterns with the seasons. At first, I laughed it off. "What am I, a bear?" But then I started thinking. Actually tracking. And damn if she wasn't right.
Every March, like clockwork, I'd feel this surge of energy. Not quite full-blown mania, but close enough to make me nervous. I'd start seventeen projects, convince myself I needed a complete career change, and suddenly find sleep utterly unnecessary. By November? Different story. The world would turn gray around the edges, and getting out of bed felt like climbing Mount Everest in flip-flops.
Turns out, I'm far from alone in this. Tons of people with bipolar disorder dance to nature's rhythm whether they want to or not. Winter depression, spring mania—it's almost cliché, except when you're living it. Then it's just exhausting.
Here's the thing about light therapy that nobody tells you upfront: if you've got bipolar disorder, that innocent-looking light box might as well be playing with fire. Sure, it can help with the winter blues, but crank it up too much or use it at the wrong time? Hello, unexpected trip to Maniaville, population: you.
I learned this the hard way. Bought a fancy light therapy lamp, thinking I'd outsmart my winter depression. Two weeks later, I was reorganizing my entire apartment at 3 AM and composing what I was absolutely certain would be the next great American novel. (Spoiler alert: it wasn't.)
Now I work with my doctor to adjust things gradually. We start tweaking my meds in early October, before the darkness really sets in. Come February, we're already planning for spring's potential chaos. It's like preparing for a storm you know is coming—you can't stop it, but you can sure as hell batten down the hatches.
The Technology Factor: Digital Age Challenges and Opportunities
Let's be honest about something: Instagram during a depressive episode is basically self-torture with a side of FOMO. There you are, unable to shower, and Karen from high school is posting her fourteenth "blessed mama" photo of the week. Meanwhile, during hypomania? That same app becomes a confessional booth where you share every profound thought that crosses your mind at 2 AM. (Pro tip: your profound thoughts at 2 AM are rarely as profound as you think.)
I've had to get real with myself about social media. When I'm spiraling down, watching everyone else's highlight reels just adds weight to the anchor. But here's what nobody prepared me for—the hypomanic oversharing. One spring, I live-tweeted my entire emotional breakdown, complete with poetry I thought was genius. My friends were concerned. My boss was... less than thrilled.
That said, I'd be lying if I said technology hasn't saved my ass more than once. There's this bipolar support group I found on Reddit where people actually get it. No judgment when you post about crying over a commercial for paper towels. No shocked faces when you mention spending your rent money on art supplies you'll never use. Just a bunch of people saying, "Yeah, been there. It sucks. Here's what helped me."
And mood tracking apps? Game changer. Though fair warning—they're only helpful if you actually remember to use them. During depression, I forget they exist. During hypomania, I'm too busy revolutionizing my entire life to bother with data entry. But during those stable periods? That's when I can look back and spot patterns I'd never noticed before.
The trick is being intentional about it all. I've had to set some ground rules for myself. No social media after 10 PM (that's when the comparison monster comes out to play). Unfollow accounts that make me feel like garbage. Follow more people who talk honestly about mental health struggles. Use those website blockers when I know I'm vulnerable to hypomanic Amazon sprees. (Did I really need seven different types of specialty salt? No. No, I did not.)
The Financial Reality: Managing Money Across Mood States
Let's talk about something that often gets overlooked: the financial impact of bipolar disorder. It's not just about treatment costs, though those can be substantial. It's about the financial chaos that mood episodes can create.
During manic or hypomanic episodes, impulsive spending can devastate carefully built savings. Grand business ideas might lead to risky investments. The absolute certainty that you've found the perfect get-rich-quick scheme can override years of financial prudence. Then depression hits, and along with everything else, there's the crushing weight of financial consequences to face.
Developing financial safeguards during stable periods is crucial. This might mean setting up automatic transfers to savings accounts you can't easily access, giving a trusted person temporary control over credit cards during warning signs of mania, or working with a financial advisor who understands your condition. Some people find that having a "mood episode fund"—money specifically set aside for the financial impacts of mood swings—reduces anxiety and provides a safety net.
Children and Bipolar Disorder: The Family Dynamic
When a parent has bipolar disorder, the entire family system is affected. Children might not understand why Mom is too tired to play this month when last month she was planning elaborate adventures. They might internalize a parent's depression as rejection or feel responsible for "fixing" their parent's mood.
Age-appropriate honesty tends to work best. Young children need simple explanations: "Mommy has an illness that makes her very tired sometimes, but it's not your fault and I still love you very much." Older children can understand more complex explanations and often benefit from learning that their parent is actively working on managing their health.
The unpredictability of bipolar disorder can actually foster resilience in children when handled well. They often develop empathy, adaptability, and emotional intelligence beyond their years. The key is ensuring they don't take on inappropriate responsibility for their parent's wellbeing and that they have their own support systems in place.
Cultural Considerations: Bipolar Disorder Across Different Communities
Mental health stigma exists everywhere, but it takes different forms in different cultures. In some communities, bipolar disorder might be seen as a spiritual issue rather than a medical one. In others, the shame associated with mental illness prevents people from seeking help until crises occur.
Language barriers can complicate diagnosis and treatment. The words used to describe mood episodes might not translate directly, and cultural expressions of emotion vary widely. What looks like mania in one culture might be considered appropriate enthusiasm in another.
Finding culturally competent mental health care can be challenging but crucial. Treatment that ignores cultural context is less likely to succeed. This might mean incorporating family in ways that wouldn't be typical in Western therapy, respecting religious or spiritual frameworks while pursuing medical treatment, or understanding how cultural values about independence versus interdependence affect treatment goals.
The Substance Use Trap: Self-Medication and Its Consequences
The relationship between bipolar disorder and substance use is complicated and often devastating. Studies suggest that more than half of people with bipolar disorder will struggle with substance use at some point. This isn't about weakness or moral failing—it's about desperate attempts to manage intolerable symptoms.
During depression, alcohol might temporarily numb the pain. During mania, stimulants might seem to enhance the high. Cannabis might feel like it smooths out mood swings. But these substances ultimately destabilize mood further, interfere with prescribed medications, and can trigger severe episodes.
Breaking free from substance use while managing bipolar disorder requires integrated treatment addressing both conditions simultaneously. It's not enough to get sober without addressing mood symptoms, nor can mood be effectively stabilized while actively using substances. The journey is challenging but possible, and many people find that sobriety actually makes their bipolar disorder more manageable than they ever imagined.
Looking Forward: Building a Life Worth Living
The narrative around bipolar disorder is changing. Where once the diagnosis felt like a life sentence, many now see it as a challenging but manageable condition. This shift isn't about minimizing the real difficulties—it's about recognizing that those difficulties don't have to define or limit a person's entire life.
Success with bipolar disorder often means redefining what success looks like. Maybe it's not about climbing the corporate ladder but finding meaningful work with flexibility. Perhaps it's not about being the life of every party but cultivating a small circle of understanding friends. It might mean accepting that some days will be harder than others while trusting that better days will come.
The most powerful stories often come from those who've found unexpected gifts within their struggles. The depth of emotion that comes with bipolar disorder, while sometimes overwhelming, can also lead to profound connections with others. The experience of rebuilding after episodes can foster a resilience that serves well in all areas of life. The intimate knowledge of both darkness and light can create wisdom and compassion that enriches not just your own life but the lives of those around you.
